Tachypnea Is Characterized By More Than ________ Breaths Per Minute.
pythondeals
Nov 16, 2025 · 11 min read
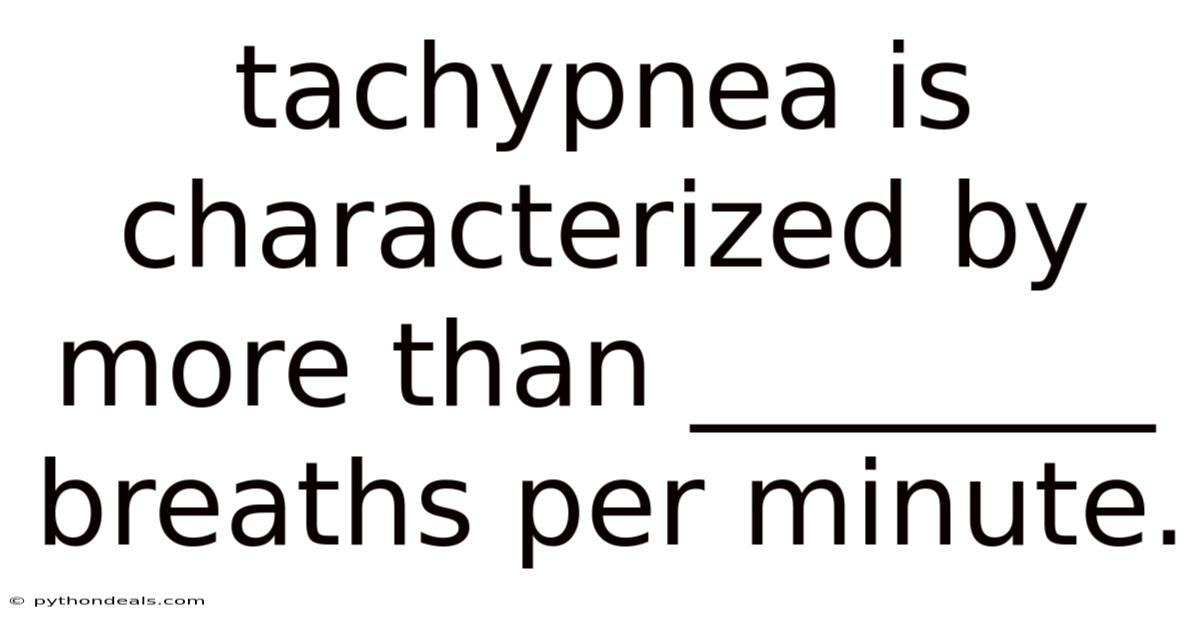
Table of Contents
Tachypnea, a term derived from the Greek words tachys (fast) and pneo (to breathe), signifies an abnormally rapid rate of breathing. It's a clinical sign, not a disease in itself, and often points to underlying respiratory or non-respiratory issues. Defining "more than ________ breaths per minute" is crucial for diagnosing tachypnea, but the specific threshold varies with age, physiological state, and even the clinical context. In this comprehensive article, we'll delve into the definition, causes, diagnosis, and management of tachypnea, with particular attention to the age-related thresholds that define this condition. We will also explore the potential underlying conditions that can trigger tachypnea and outline the steps needed to accurately diagnose and manage it.
Introduction: Understanding Tachypnea
Imagine a marathon runner nearing the finish line, their breath coming in short, rapid gasps. This is a physiological response to increased oxygen demand. Now, picture someone resting comfortably, yet exhibiting the same rapid breathing pattern. This scenario raises concern for potential underlying medical conditions. Tachypnea bridges the gap between normal physiological responses and pathological states, necessitating careful assessment.
Tachypnea isn't just about the speed of breathing; it’s also about the depth. Rapid, shallow breaths are far less efficient at oxygenating the blood than slower, deeper breaths. Therefore, understanding the context of tachypnea – the patient's age, overall health, and other symptoms – is critical for accurate diagnosis and management.
Defining Tachypnea: Age-Specific Respiratory Rate Thresholds
The critical question is: "Tachypnea is characterized by more than ________ breaths per minute." The answer isn't a single number. It depends on age, because normal respiratory rates change significantly throughout the lifespan. Here's a breakdown:
-
Newborns (0-1 month): Normal respiratory rate is typically between 30-60 breaths per minute. Tachypnea is generally defined as more than 60 breaths per minute.
-
Infants (1-12 months): Normal respiratory rate ranges from 24-30 breaths per minute. Tachypnea is defined as more than 50 breaths per minute. Some sources may use a slightly lower threshold of >40 breaths/minute, especially at the upper end of this age range.
-
Children (1-5 years): Normal respiratory rate is around 20-30 breaths per minute. Tachypnea is usually defined as more than 40 breaths per minute.
-
Children (6-12 years): Normal respiratory rate slows down to 12-20 breaths per minute. Tachypnea is defined as more than 30 breaths per minute.
-
Adults (12+ years): Normal respiratory rate is 12-18 breaths per minute. Tachypnea is generally defined as more than 20 breaths per minute.
It's crucial to remember that these are general guidelines. Individual variations exist, and clinical judgment is always paramount. Factors like anxiety, crying (in children), recent exertion, and even body temperature can temporarily increase respiratory rate.
Comprehensive Overview: Causes of Tachypnea
Tachypnea arises from a variety of underlying causes, broadly categorized into respiratory, cardiac, metabolic, and neurological factors. Understanding these potential causes is vital for effective diagnosis and treatment.
-
Respiratory Causes:
- Pneumonia: Infection of the lungs causing inflammation and fluid accumulation, hindering gas exchange.
- Asthma: Chronic inflammatory airway disease causing bronchospasm, mucus production, and airflow limitation.
- Bronchiolitis: Common viral infection in infants causing inflammation and obstruction of the small airways.
- Chronic Obstructive Pulmonary Disease (COPD): Progressive lung disease characterized by airflow limitation, often caused by smoking.
- Pulmonary Embolism (PE): Blood clot in the pulmonary arteries, obstructing blood flow to the lungs.
- Pneumothorax: Air accumulation in the pleural space, collapsing the lung.
- Pleural Effusion: Fluid accumulation in the pleural space, compressing the lung.
- Acute Respiratory Distress Syndrome (ARDS): Severe lung injury leading to widespread inflammation and fluid leakage into the alveoli.
- Foreign Body Aspiration: Obstruction of the airway by a foreign object.
-
Cardiac Causes:
- Congestive Heart Failure (CHF): Heart's inability to pump enough blood to meet the body's needs, leading to fluid buildup in the lungs (pulmonary edema).
- Pericardial Effusion/Tamponade: Fluid accumulation around the heart, compressing it and impairing its function.
- Arrhythmias: Irregular heart rhythms that can lead to reduced cardiac output and subsequent tachypnea.
-
Metabolic Causes:
- Diabetic Ketoacidosis (DKA): Severe complication of diabetes characterized by high blood sugar and ketone levels, leading to metabolic acidosis and compensatory tachypnea (Kussmaul breathing).
- Sepsis: Systemic inflammatory response to infection, causing widespread physiological changes including increased respiratory rate.
- Anemia: Low red blood cell count, reducing oxygen-carrying capacity and stimulating increased breathing rate.
- Thyrotoxicosis: Overactive thyroid gland, leading to increased metabolic rate and oxygen demand.
- Metabolic Acidosis: Build-up of acid in the body, stimulating the respiratory center to increase ventilation and eliminate carbon dioxide.
- Renal Failure: Build-up of toxins in the body can stimulate the respiratory center.
-
Neurological Causes:
- Stroke: Damage to the brain can affect the respiratory center, leading to abnormal breathing patterns.
- Brain Injury: Trauma to the brain can disrupt respiratory control.
- Meningitis/Encephalitis: Inflammation of the brain and meninges can affect respiratory function.
- Guillain-Barré Syndrome: Autoimmune disorder affecting the peripheral nerves, potentially leading to respiratory muscle weakness.
-
Other Causes:
- Anxiety/Panic Attacks: Psychological distress can trigger hyperventilation and tachypnea.
- Pain: Severe pain can stimulate the respiratory center.
- Fever: Elevated body temperature increases metabolic rate and oxygen demand.
- Medications: Certain medications can have tachypnea as a side effect.
- High Altitude: Reduced oxygen availability at high altitudes stimulates increased breathing rate.
Tren & Perkembangan Terbaru: Emerging Research and Clinical Insights
The study of tachypnea is constantly evolving, with new research shedding light on its underlying mechanisms and improving diagnostic and therapeutic approaches.
- Advanced Imaging Techniques: Advancements in CT scanning and MRI are allowing for earlier and more accurate detection of lung pathologies contributing to tachypnea.
- Biomarkers: Research is focusing on identifying specific biomarkers in the blood that can differentiate between various causes of tachypnea, potentially allowing for faster and more targeted treatment. For example, procalcitonin levels can help differentiate between bacterial and viral pneumonia.
- Non-Invasive Ventilation (NIV): NIV is increasingly used as a first-line treatment for respiratory distress, including tachypnea, avoiding the need for intubation in some cases.
- Telemedicine: Telemedicine is playing an increasing role in monitoring patients with chronic respiratory conditions, allowing for early detection and management of tachypnea exacerbations.
- Personalized Medicine: Researchers are exploring how genetic factors can influence an individual's susceptibility to respiratory diseases that cause tachypnea, paving the way for personalized treatment strategies.
- Impact of Air Pollution: Studies are increasingly demonstrating the impact of air pollution on respiratory health, linking it to increased rates of respiratory infections and exacerbations of chronic lung diseases, ultimately contributing to tachypnea.
Diagnosis of Tachypnea: A Step-by-Step Approach
Diagnosing the underlying cause of tachypnea requires a systematic approach involving a thorough history, physical examination, and appropriate investigations.
-
History:
- Chief Complaint: Document the patient's primary complaint, including the onset, duration, and severity of tachypnea.
- Medical History: Gather information about pre-existing medical conditions, medications, allergies, and past hospitalizations.
- Social History: Inquire about smoking history, alcohol consumption, drug use, and occupational exposures.
- Family History: Determine if there is a family history of respiratory or cardiac diseases.
- Associated Symptoms: Ask about other symptoms such as cough, shortness of breath (dyspnea), chest pain, fever, wheezing, and sputum production.
-
Physical Examination:
- Vital Signs: Measure respiratory rate, heart rate, blood pressure, temperature, and oxygen saturation.
- General Appearance: Assess the patient's level of consciousness, posture, and overall appearance.
- Respiratory System: Observe chest movements, auscultate lung sounds (wheezing, crackles, diminished breath sounds), and look for signs of respiratory distress (nasal flaring, retractions, use of accessory muscles).
- Cardiovascular System: Auscultate heart sounds (murmurs, gallops), assess for edema, and check peripheral pulses.
- Other Systems: Examine other systems as indicated by the patient's history and physical findings.
-
Investigations:
- Pulse Oximetry: Non-invasive measurement of oxygen saturation in the blood.
- Arterial Blood Gas (ABG): Measures blood pH, partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), and bicarbonate levels.
- Chest X-Ray: Imaging study of the lungs to identify pneumonia, pneumothorax, pleural effusion, or other abnormalities.
- Complete Blood Count (CBC): Measures red blood cell count, white blood cell count, and platelet count.
- Basic Metabolic Panel (BMP): Measures electrolytes, glucose, and kidney function.
- Electrocardiogram (ECG): Records the electrical activity of the heart to detect arrhythmias or other cardiac abnormalities.
- Sputum Culture: Identifies bacteria or other organisms in the sputum.
- Pulmonary Function Tests (PFTs): Measures lung volumes and airflow to assess lung function.
- CT Scan of the Chest: More detailed imaging study of the lungs, used to evaluate for pulmonary embolism, lung masses, or other abnormalities.
- D-dimer: Blood test used to rule out pulmonary embolism.
- Echocardiogram: Ultrasound of the heart to assess heart function.
The specific investigations ordered will depend on the suspected underlying cause of the tachypnea.
Treatment of Tachypnea: Addressing the Root Cause
Treatment of tachypnea is directed at addressing the underlying cause. The following are some general principles:
- Oxygen Therapy: Administer oxygen to maintain adequate oxygen saturation.
- Medications:
- Bronchodilators: Used to open airways in patients with asthma or COPD.
- Antibiotics: Used to treat bacterial infections such as pneumonia.
- Diuretics: Used to reduce fluid buildup in patients with congestive heart failure.
- Pain Medications: Used to relieve pain that may be contributing to tachypnea.
- Respiratory Support:
- Non-Invasive Ventilation (NIV): CPAP or BiPAP can provide respiratory support without the need for intubation.
- Mechanical Ventilation: Intubation and mechanical ventilation may be necessary in severe cases of respiratory distress.
- Other Treatments:
- Thoracentesis: Removal of fluid from the pleural space in patients with pleural effusion.
- Chest Tube Placement: Insertion of a tube into the pleural space to drain air or fluid in patients with pneumothorax or pleural effusion.
- Anticoagulation: Treatment with blood thinners in patients with pulmonary embolism.
Tips & Expert Advice: Practical Strategies for Managing Tachypnea
As healthcare professionals, we can offer the following advice:
- Early Recognition is Key: Promptly identify tachypnea and assess for signs of respiratory distress. Don't dismiss it as "just anxiety" without a thorough evaluation.
- Accurate Respiratory Rate Measurement: Ensure accurate measurement of respiratory rate. Count breaths for a full minute, especially in infants and children.
- Consider Age-Specific Norms: Always consider age-specific normal respiratory rates when assessing tachypnea.
- Look for Underlying Causes: Focus on identifying the underlying cause of the tachypnea. Don't just treat the symptom.
- Monitor Oxygen Saturation: Continuously monitor oxygen saturation and adjust oxygen therapy as needed.
- Provide Supportive Care: Ensure patient comfort and provide supportive care, such as positioning and anxiety management.
- Communicate Effectively: Communicate clearly with patients and their families about the diagnosis, treatment plan, and prognosis.
- Document Thoroughly: Document all findings, interventions, and patient responses in the medical record.
- Consult Specialists: Don't hesitate to consult with pulmonologists, cardiologists, or other specialists as needed.
- Stay Up-to-Date: Keep up-to-date with the latest research and guidelines for the management of tachypnea.
FAQ (Frequently Asked Questions)
-
Q: Is tachypnea always a sign of a serious medical condition?
- A: Not always. It can be caused by benign conditions such as anxiety or fever. However, it's important to rule out serious underlying causes.
-
Q: Can tachypnea be treated at home?
- A: It depends on the underlying cause. Mild cases may be managed at home with rest and supportive care, but more severe cases require medical attention.
-
Q: What is the difference between tachypnea and hyperventilation?
- A: Tachypnea refers to an increased respiratory rate, while hyperventilation refers to breathing that is deeper and/or faster than normal, leading to a decrease in carbon dioxide levels in the blood. While tachypnea can be a component of hyperventilation, the terms aren't interchangeable.
-
Q: What are the long-term effects of tachypnea?
- A: The long-term effects depend on the underlying cause. Chronic respiratory diseases can lead to long-term complications.
-
Q: When should I seek medical attention for tachypnea?
- A: Seek immediate medical attention if you experience tachypnea accompanied by shortness of breath, chest pain, dizziness, confusion, or loss of consciousness.
Conclusion
Tachypnea, characterized by a respiratory rate exceeding age-specific norms (more than 60 breaths per minute in newborns, more than 50 in infants, more than 40 in young children, more than 30 in older children, and more than 20 in adults), is a significant clinical sign that warrants thorough investigation. Understanding the potential underlying causes, from respiratory infections to cardiac conditions and metabolic disturbances, is crucial for accurate diagnosis and effective management. By employing a systematic approach involving a comprehensive history, physical examination, and appropriate investigations, healthcare professionals can identify the root cause of tachypnea and implement targeted treatment strategies. Early recognition, accurate assessment, and prompt intervention are essential for improving patient outcomes and preventing long-term complications.
How do you approach assessing respiratory distress in your clinical practice? What are some of the most challenging cases of tachypnea you've encountered?
Latest Posts
Latest Posts
-
What Is A Negative Control In An Experiment
Nov 16, 2025
-
What Are The Steps For Dna Fingerprinting
Nov 16, 2025
-
Which Example Is A Trace Fossil
Nov 16, 2025
-
What Part Of Speech Is About
Nov 16, 2025
-
How To Prove Linear Independence Of Vectors
Nov 16, 2025
Related Post
Thank you for visiting our website which covers about Tachypnea Is Characterized By More Than ________ Breaths Per Minute. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.